As part of her improvement project exploring how to increase capability to deliver continuous quality improvement, she shares her thoughts Sweden's approach to health and care systems.
One of the places I knew that I wanted to visit was Jonkoping in Sweden. I had seen a few presentations and read about how Jonkoping Region had made quality improvement their organising principle; and how this had really changed the way they went about large-scale service transformation.
A two-day visit at the beginning of December was arranged, with some trepidation about how cold and snowy it would be. I went prepared with my woolly hat and scarf! Surprisingly it was no colder than at home. Agata Rukat, Quality Improvement Advisor had very kindly arranged a packed and varied agenda for me to meet people who could share with me the work they had done and some of the lessons they had learnt along the way.
As I walked up to the front doors on a cold, dark and wet December morning, I was greeted with the view of the Qulturum. I almost expected it to sparkle like Cinderella’s castle on the Disney films as this is a place as magical as Disney if you’re interested in quality improvement.
Seven Reflections
Permission to innovate was a strong theme and using small tests of change to try things, it isn’t an issue if it doesn’t work but there is an expectation that everyone is trying to improve what they do. James Dyson made over 5000 iterations of the first Dyson vacuum cleaner before he got a product that worked, yet the NHS often decides on large scale change with very little opportunity to test it out and get it right before we have made huge structural and workforce changes, by which time there is no going back.
1. Our problems are similar, our solutions aren’t
Sweden; like the UK is a tax funded system and as such is suffering from similar financial and operational pressures. The shortage of clinical staff, particularly doctors and nurses is not confined to the UK and this has forced Sweden to think differently. This is one of the main differences between Sweden and the UK in that we have the same problems but they have innovated differently. Anyone who has been in an IKEA store can see the innovation and thinking about the box differently, never mind thinking outside of it. They are braver than we are.
Permission to innovate was a strong theme and using small tests of change to try things, it isn’t an issue if it doesn’t work but there is an expectation that everyone is trying to improve what they do. James Dyson made over 5000 iterations of the first Dyson vacuum cleaner before he got a product that worked, yet the NHS often decides on large scale change with very little opportunity to test it out and get it right before we have made huge structural and workforce changes, by which time there is no going back.
2. Different folks, different strokes
The staff at the Qulturum all come from different occupational backgrounds and from many different nations. This brings together a plethora of knowledge and experience, both professionally and personally. I felt strongly that these divergent thoughts are one of the reasons the solutions work so well as they all bring a different perspective to a problem.
3. Patience and time
“The two most powerful warriors are patience and time” – Leo Tolstoy.
This is not to say that people can just say that things take time to change and you’ll have to be patient. There is a lot of activity in making those changes but there is an acknowledgement that change doesn’t happen overnight.There is an understanding that the human side of change is messy and less predictable and space is given for people to accept and welcome change and be actively involved in the decisions about the direction of that change. Data used intelligently and not just to demonstrate outcomes helps to reflect on the progress and show that changes are taking place.
This is not to say that people can just say that things take time to change and you’ll have to be patient. There is a lot of activity in making those changes but there is an acknowledgement that change doesn’t happen overnight.There is an understanding that the human side of change is messy and less predictable and space is given for people to accept and welcome change and be actively involved in the decisions about the direction of that change. Data used intelligently and not just to demonstrate outcomes helps to reflect on the progress and show that changes are taking place.
4. Co-production

Jonkoping is recognised for its ability to co-create services that patients and staff want and need. As well as co-creating care with patients/citizens they have co-created care systems with the staff who work in them to give them joy in work by combining a number of methods of improvement such as LEAN, clinical microsystems and model for improvement. They haven’t been afraid to take different methods and use them where they will work well- there is no thought that you cannot use a process map because you are not a LEAN practitioner or you are also using experience based design as part of the same improvement project.
One of the most inspirational people I met, (high praise indeed as everyone was inspirational!) was Patrick Blomqvist. Patrick is one of the patient supporters for the region, in fact I would say he is THE patient supporter. Patrick has in his own words been a “hostage” of the healthcare system over many years and particularly when the health services started to include patients in designing services. Much of this patient involvement was in a tick box way so organisations could say they had consulted with patients. Patrick would be the token, single patient representative and his views would be listened to but not necessarily heard. Perhaps the 2 most famous of Jonkoping’s co-produced and patient led projects are self haemodialysis for patients with kidney failure and the Esther programme.
Self Dialysis Unit
For many health professionals the thought of letting patients have responsibility for such a complex, life saving treatment may sound the worst idea in the world but for Jonkoping that is exactly what they have done; with international recognition following. Supporting patients to help themselves has not only reduced their physical side effects but has improved infection rates and increased both staff and patient satisfaction. This all began by a person who wasn’t prepared to just be a condition and a nurse who felt that they had permission to think about the care they provided in a different way by seeing the patient as a person and a partner in their care.
“Person centred care is to see and meet the whole person. The person’s story is the starting point for the partnership, joint planning and mutual respect for each other knowledge” Patrick Blomqvist, Patient Supporter
Esther
No one would argue; that as health professionals we all believe that we are doing our best for our patients, but often we do this in isolation of each other and most importantly without real consideration of whether it is the best for the patient and what the patient wants. Often patients feel they are lost in the system.
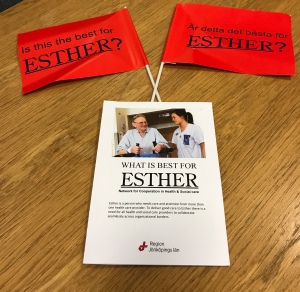
The Esther programme has trained Esther coaches around the world to think differently about ensuring the patient is at the centre of the care, by training them in person centred care, quality improvement techniques and systems thinking. The programme encourages them to think about the actions in the system that go on to the left and the right of their intervention to make the system interlock and work as a system, reduce the repetition and the permission to redesign with the patient and for the patient. The programme is so successful there is an annual Esther Day in Sweden and the programme has been replicated across the world.
5. Always learning, always curious
The Qulturum collaborates with various organisations, perhaps the 2 most high profile being the Institute for Healthcare Improvement (IHI) and the Dartmouth Clinical Microsystems Academy. These critical friends help to support a culture of innovation and constant questioning that allows the Qulturum to develop its own message that, although influenced by many different areas of study and knowledge is synthesised into its own.
I was surprised by the curiosity that the people I met showed to the work we are doing and as much as I wanted to learn from them they were keen that I shared my work in the hope that they could learn from some of our good practice. This curiosity wasn’t confined to my work though. They have renamed the study tours to co-learning visits as they feel they learn as much from their visitors as their visitors do from them.
This curiosity and learning extends out from public services that the region has responsibility for to commercial organisations to understand what can translate to the services that the region are responsible for. Everyone at the Qulturum was deservedly proud of the work and the difference their individual work programmes made and the work of the Qulturum as a whole. They were also very humble and felt that even though they had achieved much there was still lots to do and lots to learn.
I was surprised by the curiosity that the people I met showed to the work we are doing and as much as I wanted to learn from them they were keen that I shared my work in the hope that they could learn from some of our good practice. This curiosity wasn’t confined to my work though. They have renamed the study tours to co-learning visits as they feel they learn as much from their visitors as their visitors do from them.
This curiosity and learning extends out from public services that the region has responsibility for to commercial organisations to understand what can translate to the services that the region are responsible for. Everyone at the Qulturum was deservedly proud of the work and the difference their individual work programmes made and the work of the Qulturum as a whole. They were also very humble and felt that even though they had achieved much there was still lots to do and lots to learn.
6. Measure, measure, measure!
Measurement is nearly always one of the parts of improvement work that people dislike the most but it is essential as without it; how do you know you have improved. I know it is one of the aspects of improvement I struggle to engage people with as it is often seen as lots of numbers and graphs. One of the things I learnt in Jonkoping was that we need to pay more attention to making people measurement and data literate. Also that as we do with clinical information we should alter the way in which the data is presented depending on the audience that will be receiving it. Often we don’t ask people what information they want so they can understand if a change is an improvement. We need to move away from data for management, the NHS is awash with data but very little of it is used for improvement, this is a place we need to go to understand fully what works and what doesn’t.
7. Quality improvement is in their DNA
Quality improvement science teaching runs through all the education programmes. They have made quality improvement the method of change, their organising principle and business planning strategy. As part of leadership programmes people have to complete QI projects, patient supporters are taught quality improvement, Esther coaches are taught quality improvement, patient safety improvements are rooted in quality improvement science. Quality improvement is taught in simulation and is practiced by those who lead the simulation centre by always looking at better ways of delivering the training and better ways of storing all their kit – I can’t imagine anyone else has a storage system for the simulation mannequins that is quite the same, it looks very similar to a mortuary fridge but includes all the connections for keeping the mannequins “alive”, truly unique and a testament to their quality improvement ethos.

Data collection and understanding data is imperative as part of any change that anyone wants to make – you have to be able to see the journey that has been made. The expectations on anyone in a leadership position at any level is that they will increase capability and capacity in their sphere of influence and the quality improvement knowledge and skills are just as important as the technical and clinical skills of a role.
It was a packed two days and these reflections only give a sense of the learning and sharing I was fortunate enough to participate in. The overwhelming take-home message was, don’t be afraid to try something that might not be what everyone expects, but with that make sure you co-create this with those people who it directly affects, both staff and patients, quality improvement should be the organising principle of all you do. Think more widely and creatively about what data for improvement is and how to make sure it is displayed and explained in a way that connects with the audience.
The answer to the question, Has Sweden got more to share than Ikea and Abba? The answer is a resounding yes.
I do think there are some parallels between the solutions that Ikea have developed – particularly innovative space-saving solutions and the solutions that Jonkoping Region have developed. Agnetha Faltskog was born in Jonkoping and as a founding member of ABBA has given many of us joy; and joy in work is one of the key elements of Jonkoping’s strategy. I think innovation and joy are in the country’s DNA, not just Jonkoping’s.
I would like to express my sincere and heartfelt thanks to everyone at the Qulturum who kindly and willing shared their time, knowledge and learning with me. It will be well used!
Feel free to share your thoughts with Caroline on Twitter via @Cargreenhalgh or via @AQuA_NHS. For more information about AQuA's Leadership for Improvement Fellows, please visit our website.
This blog was originally published on Caroline's Quality Improvement Journey blog.


By all means make the patient room environment as clean and silent as possible, communicate effectively with the patient, and ensure that they are fully prepared to be discharged, but the emphasis must still be on the patient's perception. moe's diabetic
ReplyDelete